MicroSurgical Endodontics (Apicoectomy)
Surgical endodontics plays an important part of an endodontic practice.
It is a skill that needs to be developed carefully, with proper training and understanding of the surgical guidelines.
In this blog post I would like to talk somewhat briefly on the guidelines or surgical indications that we follow and perhaps in future blog posts I can reviews microsurgery in more detail.
Our office philosophy for the most part is focused on root disinfection, and for that reason we would consider ourselves to be (generally speaking) retreatment focused before consideration for apicoectomy procedures. However the surgical approach is necessary in many conditions.
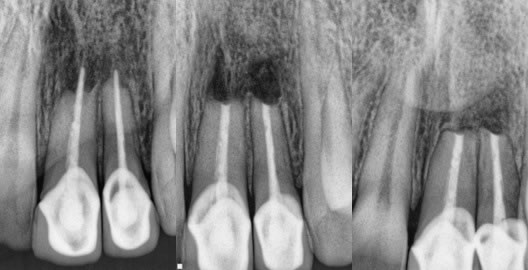
1. Thick or deeply set posts with well made coronal restorations. (figures 1-3)
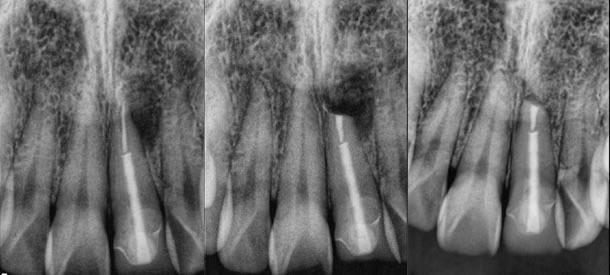
Figures 1-3: pre-op / post-op / 9 months healing recall
Original root canal therapy performed by another endodontist and the crown was so perfect and the post deeply set. I performed the surgery on my friend with a great result.
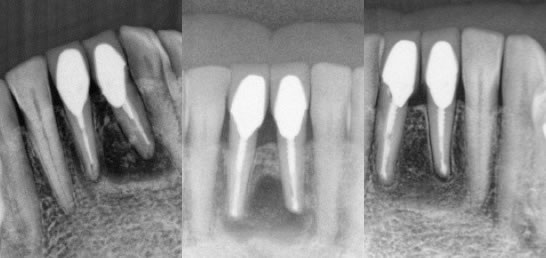
2. Very well done original endodontic therapies.
These would often be scenarios to which we know the specific history of the original root canal treatment, such as treatment that we had originally provided. (figures 4,5) (figures 6,7,8)
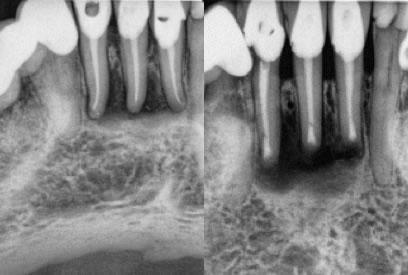
Figures 4-5: pre-op / immediate post-op
Original RCT’s performed by myself, but lesions never healed after 2 years and thus apicoectomy performed just a couple months ago. I do not have a long enough recall at this point, but the buccal fistula has fully healed.

Figures 6,7,8: pre-op / post-op / 14 month recall
Original RCT performed by myself and a lesion developed 2 years later. I of course knew this case well and that the tooth was treated in a multi-visit approach using calcium hydroxide. I felt apicoectomy would be a more definitive approach and the healing has been excellent.
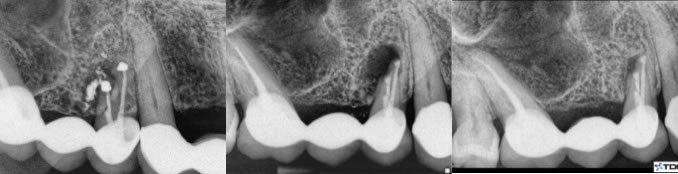
3. Extreme conditions of calcification that made perfect root canal treatment impossible. (figures 9,10,11)
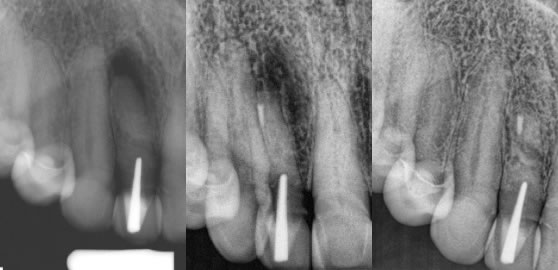
Figures 9,10,11: pre-op / post-op / 1.5 year recall
Original root canal effort done by a highly skilled endodontist who could not find the extremely calcified canal and the post/crown complex was very esthetic. Patient did not want it removed and thus I performed the apicoectomy with a very nice result.
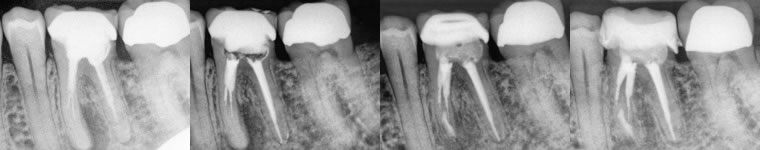
4. Severe canal transportation by original root canal therapy that would make retreatment impossible. (figures 12,13,14)

Figures 12,13,14: pre-op / post-op / 6 month recall
In this case there was a transported canal in combination with a large post. Therefore, surgery made a lot of sense rather than full dis-assembly of the crown/post complex with potentially very limited upside on the retreatment. I performed conventional treatment on #14 and apicoectomy on #13 and the healing looks great after just 6 months.
5. Separate instruments that would prevent retreatment endodontics. (figures 15,16,17,18)
Figures 15,16,17,18: pre-op / post-op retreatment / post-op apicoectomy / 13 month recall
I performed retreatment endodontics first with hope of bypassing/removing the separated instruments in the mesial canals. I was only able to retreat the distal canal and then performed apicoectomy on the mesial canals. He has been asymptomatic and comfortable since treatment.
6. Various Unique cases that I simply categorize as something different. (figures 19,20,21) and (figures 22,23,24)
Figures 19,20,21: pre-op / post-op / 5 month recall
Significant root-end resorption. I did see the original RCT performed by a previous endodontist and the gutta percha was exactly to the root end, thus the resorption has occurred after the RCT was completed. The coronal restorations were great and so I performed apicoectomy in this case. The healing was nearly complete at just 5 months.
Figures 22,23,24: pre-op / post-op / 6 month recall
My patient told me she had 3 RCT’s on each tooth and 2 sets of crowns over the past 20 years on the teeth. I had actually recommended retreatment again because the RCT’s were inadequate, but she was not at all interested in anything other than the least amount of hassle and treatment since she had been through so much already. I performed the apicoectomy on both teeth and she reported her teeth have never felt this good in 20 years.
7. Previous Apicoectomy treatments that have had an infection recurrence. (figures 25,26,27)
Figures 25,26,27: pre-op / post-op / 14 month recall
This patient came to me understanding from her referring dentist that there is likely not much to be done and the bridge will be lost. Retreatment endodontics is not indicated and we decided to do what we can to save this bridge vs. bridge removal, extraction, implant, possible sinus lift, etc. The apicoectomy approach is far less involved and resulted in saving this bridge.
The above cases are a few of the good indications for microsurgical endodontics, but I’m sure there are a number of other conditions that are very suitable for apicoectomy. The important part is to consider all treatment options and weigh the risk/benefit relationship and the pros/cons as compared to each treatment method.
I personally, and my partners here in the office, have formulated our thoughts, but even that changes over time as we continue to grow and practice and adapt to the constantly changing field of dentistry.
In a future blog post I plan to describe the microsurgical treatment method itself and provide a video of how the procedure is performed. If you have any questions let me know!
