For this weeks blog I would like to discuss extra canal invasive resorption (ECIR).
This is subject matter that is very interesting to me, mainly because I find our practice has treated a significant number of cases over the past few years involving this condition. Although the occurrence is rare within the general population (usually less than 1%), it is by far the most common type of resorption we see as endodontists.
Definition
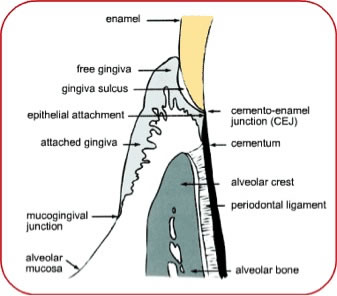
ECIR is a type of external root resorption that usually starts in the cervical region, below the epithelial attachment of any permanent tooth. Figure 1 is a cartoon of the periodontal tissues for reference.
Etiology
The development of ECIR is not well understood but it seems that a defect in the cementum is a prerequisite, whether it be from some kind of developmental imperfection (See Figure 2) or as a result of injury. This defect allows for direct contact between the dentin and certain resorptive cells in the local periodontium, resulting in an invasion of highly vascularized tissue and destruction of tooth structure.
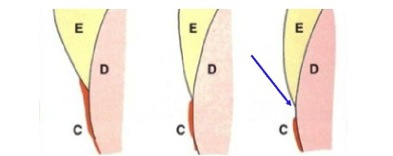
Figure 2- 60% of the population have the cementum covering the enamel at the CEJ (left). 30% have an edge to edge relationship (center). 10% have no connection between the cementum and enamel, allowing for the dentin to be exposed. This may predispose a patient to developing ECIR.
In a classic article by Heithersay (2004), 222 patients with a total of 257 teeth were analyzed and a number of predisposing factors were discussed, the most common of which were orthodontic treatment, trauma, internal bleaching and a history of surgery in the cementoenamel junction area. Orthodontic treatment (24.1% of cases) and trauma (15.1% of cases) were the most common sole factors and I find this observation to be true in most of the ECIR cases we evaluate in our office. Now of course if you have had braces and you developed an area of resorption, you should certainly NOT be angry at your orthodontist! You may just simply be an unlucky 24.1% of <1% of the population. Thankfully, if ECIR lesions are caught in their early stages, prognosis is generally good. I will discuss treatment options in next weeks blog.
Classifications
Heithersay (2004) developed a useful classification system for ECIR lesions that is defined in the Figure 3 below.
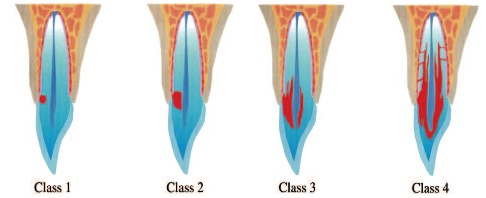
Figure 3- Classification of ECIR
Class I- Small lesion with a shallow penetration into dentin
Class II- Larger lesion extending close to the pulp chamber but not extending into the radicular dentin.
Class III- Lesion extends into the coronal third of the root.
Class IV- Lesion extends beyond the coronal third of the root.
Clinical Presentation
A major challenge with ECIR lesions is they are typically asymptomatic and difficult to discover unless they are at a class III or IV. If clinically detectable, a tooth may take on a pinkish hue near the gingival margin, due to the highly vascular inflammatory tissue that is replacing the tooth structure. There may be a cavitation that is detectible with an explorer. The tooth structure is usually hard, not sticky as is the case when detecting a carious lesion, however large lesions may also have secondary decay as a result of the defect creating a hygiene issue. Localized periodontal inflammation may also be observed for this reason as well. (Figures 5 and 6)
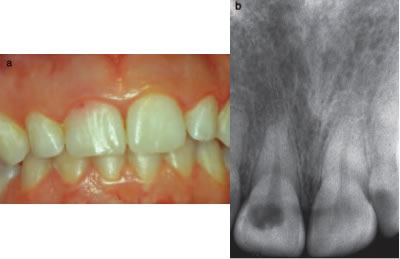
Figure 5- Small ECIR defect detectible at the gingival margin of #8. The pinkish hue of the inflammatory tissue is visible through the translucent enamel. Associated radiograph is included.
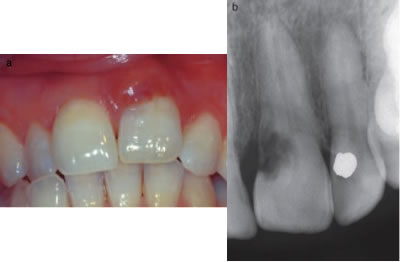
Figure 6- localized periodontal inflammation as a result of an ECIR lesion #9. Associated radiograph is included.
Radiographic Presentation
ECIR lesions are usually missed until they have reached a class III or IV status, appearing as a moth eaten radiolucency with ragged borders (Figure 7). The communication with the periodontal tissues may be pinpoint or cavernous. Larger lesions may also contain hard tissue and have a trabecular bone type appearance. The pattern of resorption is unique as it typically progresses vertically alongside the pulp without penetration(Figure 8). A thin layer of dentin and predentin usually remains intact and walls off the pulp from the invasive fibrovascualar tissue. As a result most teeth with ECIR lesions contain vital pulp tissue and periapical tissues appear normal. Again the resorption process is due to rogue clastic periodontal host cells and does not inherently involve acute or chronic inflammatory cells unless microorganisms have secondarily invaded the space.
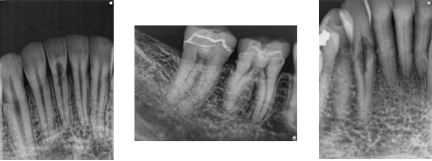
Figure 7- Radiographic appearance of ECIR. From left to right, #’s 24, 30, and 27. All cases are from patients of Tri-City Microendodontics.
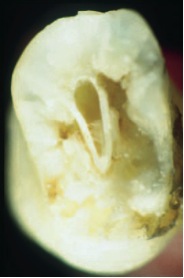
Figure 8- Tooth with Class IV ECIR sectioned at midroot. Although the resorption has lead to significant destruction of tooth structure, there is an in tact dentin/pre-dentin layer preventing perforation into the pulp.
Cone Beam Computed Tomography (CBCT) Presentation
ECIR lesions can be difficult to appreciate in 2 dimensional radiographs so we usually take a cone beam CT scan of almost every ECIR case we encounter. The CBCT is invaluable as it allows for the most accurate 3 dimensional representation of the lesion and leads to more accurate assessment, diagnosis, and treatment planning (See Figure 9). Additionally, the scan provides an excellent visual aid for patient communication and education. We spend a lot of time getting to know every patient and we make sure they understand as much as possible. This is extremely important as many times ECIR lesions are asymptomatic and it may be difficult for a patient to understand the need for treatment when there is no pain. The truth is radiographic and CBCT images are invaluable for treatment planning however they are of very little value when it comes to predicting a patient’s discomfort.
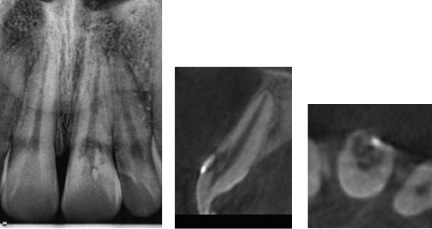
Figure 9 – Radiograph of #9 with Class III lesion (left). CBCT coronal slice (center) and axial slice (right). CBCT reveals the lesion originated on the labial surface and extends into the coronal third of the root.
Now is a good time to conclude part one. Next week in part 2, I will review treatment options, clinical procedures, and prognosis. I will also post a few recent cases from our office. Thank you for reading and see you again next week!
