A continuation of my blog from last week.
Last week I had written a simple blog on some of the indications for the apicoectomy approach. This week I wanted to continue the topic, but now breakdown and simplify the actual treatment process. And more specifically this blog post will try to outline the diagnostic and work-up process of apicoectomy as a treatment option. I will try to keep this post easy to follow rather than the heavy details of a text book, and feel free to ask us any questions you may have.
The most important part of the surgical process is in the treatment planning phase. Not all teeth are suitable for this treatment, and not all patients are good candidates for the option. Thus the proper diagnosis of the pathology and an appropriate discussion with the patient is of high importance.
I will discuss the following factors for consideration:
1. Location of the tooth as it relates to visibility and oral anatomy
2. Skill and comfort of the operator
3. Identifying and qualifying the proper periodontal condition that impacts the success rate of apicoectomy
4. Judging the expectations and character of the patient
5. Patient health considerations
1. The location of teeth as it relates to how difficult a treatment can be is certainly something we deal with in any aspect of dentistry. It’s more difficult to scale the distal-lingual line angle of #31 vs. the mesial aspect of #8. It’s more difficult to place a DO filling on #2 vs. a class 1 on #12. Similarly apicoectomy is extremely challenging at the distal root of #30 vs. the maxillary lateral incisor.
So as a “general” rule of thumb anterior teeth are easier to perform surgery upon than posterior teeth. What you can see, you should be able to treat. What you cannot see, you will struggle to perform.
- the exceptions could be lower anterior teeth with steep buccal inclinations thus making the root tips tilted far lingually.
- tilted teeth/rotated teeth
- maxillary canines that are extremely long
- interference of anterior nasal spine with maxillary centrals
Additionally, there are anatomical structures that must be considered with the surgical approach.
- mandibular canal
- mental foramen/nerve
- maxillary sinus
- palatal approach for palatal roots (not commonly done)
Certainly with the use of CBCT imaging allows much better selectivity when offering this treatment approach by the precision of measurements and identification of the interfering anatomy. At this point in our office we never perform an apicoectomy without a CBCT regardless of tooth location.
I will say though that while we consider ourselves to be overly safe in our selection process with regards to anatomy, I think that you might be surprised that the treatment is much safer than your original preconceptions. What I mean is that a nearby sinus is not at all an absolute contraindication (figures 1,2,3,4). Additionally, what you might think is too close for a mandibular canal is sometimes not a problem. (figure 5,6,7)

Fig 1: Pre-op #4, Fig 2: Immediate post-op #4 (completed last week)
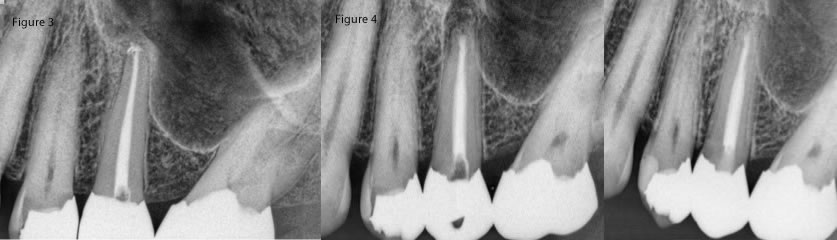
Fig 3: Pre-op #13 near sinus, Fig 4: Immediate post-op #13 and 10 month recall- fistula has not returned.

Fig 5: pre-op #19, Fig 6: immediate post-op #19, Fig 7: 2.5 year recall with complete healing
There are a host of other factors that affect visibility such as hemeostasis, appropriate flap design to exposure the surgical site, etc. Perhaps in another future blog post I will tackle those issues, but for now let us move on to the second category of this blog which is the skill and comfort of the operator.
2. This is the more subjective or personally reflective component of the decision making process. What might be comfortable for us in the office might not be as comfortable for another. Conversely we might be less comfortable in certain situations than another. We all consider ourselves skillful in the microsurgical approach, but we do have our limitations. For me, I will rarely perform surgery on a second molar. I also have declined the surgical approach for insufficient lip retraction, extreme tilting of the teeth, and a host of other conditions. What I think is important though is to assess the tooth and accurately make a self judgment of the skill set needed to perform to a very high level.
3. The third category is a critical component to consider. The periodontal status of a tooth plays a huge factor in prognosis of treatment. Simply stated; the better the periodontal support, the better the prognosis. As you can imagine a tooth with little bone support will result in a failed surgical treatment and tooth loss.
There is way to categorize the periodontium introduced by my mentor Dr. Kim (University of Pennsylvania). He has created 6 categories: A, B, C, D, E, F.
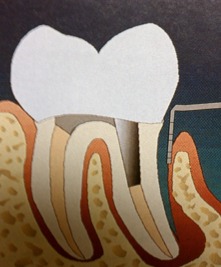
Category A and B would be defined as very good periodontal support with normal sulcular depths and buccal plate intact. Category A has no apical lesion and Category B and an apical lesion. The image below would show the surgical appearance once the tissue has been flapped.
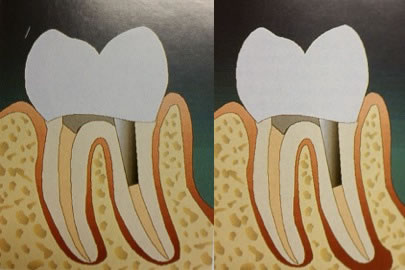
Category A and B
Surgical View
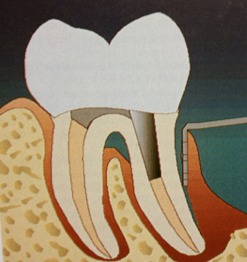
Category C has normal sulcular depth and buccal plate intact, but the apical lesion extends about half way up the root.
Category D has an apical lesion, but in this case the buccal bone starts to become compromised and the sulcular depth extends well onto the root surface.
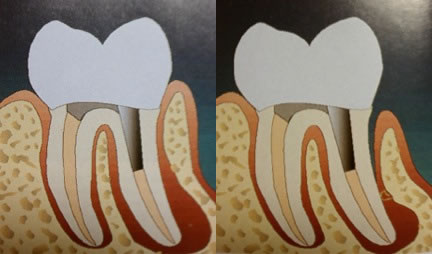
Category C and D
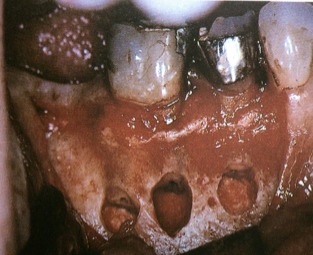
Category E is a condition where the apical pathology and the periodontal sulcus depth do join in a true combination periodontal/endodontic infection. The image below also shows the surgical view once the tissue has been flapped back.
Category E

Surgical View of a Category E
Category F is of course the worst periodontal condition for a tooth with no buccal bone at all and total attachment loss to the apex of the root. You can again see the image showing this surgical view with a total lack of buccal plate.
Category F

Surgical View of a Category F
It should be clear that category A, B will lead to the best chances for a surgical success. I also feel that category C conditions lead to predictable outcomes as well. The drop off in success really occurs most steeply at category D and the final categories of E and F should essentially be avoided entirely.
A very good examination of the tissue and probings are very important. And now that we have CBCT imaging we can certainly better assess the presence of the bone and tightness of the bone around all root surfaces leading to better decisions.
4. And this brings us to the next bullet point of the blog which is the patient assessment. Of course common to just about any dental procedure, but applying more so to the treatments generally thought to be more involved (ie. root canal therapy, surgery, extractions, implants, etc). There are times when all the first 3 bullet points of this blog are met perfectly. The tooth location and visibility are ideal, the operator feels very comfortable with the technique, and the periodontal condition is just perfect, but the patient is not of the mindset that can handle the thought of apicoectomy.
My strong feeling is that for most of these patients the primary hang up is the word “surgery”. In other words if “surgery” was not used in the description then there would be more patients open to the treatment option. Especially considering there are often alternative treatment options to choose such as retreatment or extraction/implant/bridge.
Interestingly, in my experience almost always patients will remark following completion of treatment how much easier the process was as compared to their expectations. They were numb, they could take breaks, and they could ask me questions; all of which lead to a better experience. I also strongly feel that the post-operative experience is often easier than that of retreatment. I rarely see a flare-up condition of strong pain or swelling following surgery.
Yet despite efforts to convey to a patient the experience is really quite simple, some just are not good candidates because of their own anxiety. And to those situations, microsurgical endodontics would be contraindicated.
5. The final point is the obvious and always reviewed patient health condition that should be accounted for in any situation with any treatment. But for surgery the patients health and medications need to be more closely assessed. I will leave that discussion for another time considering medical history can lead to pages and pages worth of information not particularly suitable for a simple blog post.
Hopefully this has been interesting and helpful to gain a bit more insight to just some of the things we think about in the diagnostic process.
I recently posted a video of an apicoectomy I performed on our facebook page if interested. Click HERE to view.
