CBCT Utilization During Root Canal Treatment
The following case perfectly exemplifies the importance of Cone Beam CT scanning technology during endodontic treatment.
I first met with Mrs. R on 12/20/12. She had a Zirconium crown delivered on tooth #14 (UL first maxillary molar) in the first week of December and the tooth had been sensitive to biting and chewing since then. Her general dentist made on occlusal adjustment the day before sending her to our office for an evaluation.
My clinical findings showed that in fact #14 was the only tooth sensitive to biting and percussion in the UL quadrant. All other teeth were testing within normal limits. Radiographic exam revealed no definitive evidence of periapical bone loss and infection although the pulp chamber and canals were very calcified (Figure 1). The tooth was not responding to cold, however I was concerned that the calcification and/or presence of the crown were giving me a false negative.

Figure 1: Initial PA radiograph for tooth#14. Calcified pulp system. Areas of periapical bone loss are difficult to visualize.
I explained to Mrs. R that her pain to biting and chewing (apical periodontitis) could be the result of couple of different scenarios…
1- The sensitivity to biting was a result of hyperoclussion and crown simply needed to be adjusted, a common issue for newly cemented full coverage restorations. When the crown is fitted to the opposing dentition in a balanced way, any sensitivity should gradually diminish over a period of a few weeks. The negative cold testing in this case is a false negative. The nerve is alive and well, however, as a result of the heavily calcified pulp system and the presence of the crown, I am not able to produce a normal response with a cold test. No treatment recommended.
2- The sensitivity to biting is the result of an apical periodontitis as a result of the periapical tissues responding to the presence of bacteria within the pulp system. The nerve is dead and pulp is necrotic and infected. This scenario of course requires root canal treatment to remove the bacteria from the inside of the tooth and resolve the infection.
Since the adjustment to the crown was made the day before I met Mrs. R, we decided to take a conservative approach and wait a few weeks, hoping her symptoms would resolve.
Mrs. R returned again on 1/8/13 complaining that unfortunately her symptoms had worsened. She continued to experience discomfort to biting and chewing, however the tooth was now sensitive to palpation near the apices of the MB and DB roots and she was experiencing an intermittent dull ache.
At this time we had enough evidence to suggest an endodontic diagnosis of necrotic pulp/symptomatic apical periodontitis and root canal therapy was started. I accessed through the crown and into the pulp chamber to find the pulp was necrotic and the pulp system was very calcified. MB, DB, and P canals were detected quickly and fully instrumented. There was a fin extending from the MB orifice 3mm in the palatal direction however I was unable to find a definitive MBII canal even after searching with the ultrasonic instrument.
A little side note about the ever so elusive MBII canals in first maxillary molars…the research shows they are there a majority of the time. I will take it a step further and say they are almost ALWAYS there. In fact I don’t remember the last time I treated a first maxillary molar and didn’t find one. Using microscopes on every case is a beautiful thing!
So anyway, I was disturbed by the fact I could not find the MBII and decided to take a 3 dimensional image with our Cone Beam CT scanner. The CBCT is a truly remarkable piece of equipment and offers a wealth of information, which far exceeds the diagnostic capability of traditional X-rays, either film or digital.
The scan showed a couple of important features. First of all, there were very clear periapical areas of bone loss associated with both MB and P roots (Figures 2, 4, 5, 6) . Both lesions were essentially invisible on the digital X-ray taken on 12/20/12. I find the CBCT is invaluable in certain areas of the mouth, the posterior maxillary quadrants in particular. The inherent complex nature of the localized anatomy (multi-rooted teeth, zygoma, inferior border of the maxillary sinus) can be easily misrepresented when you “squash” the area into 2 dimensions by taking a periapical x-ray. Secondly, it appeared that the MB root was, in cross section shaped in a way that suggested the presence of an MBII (Figure 3).
(Click on thumbnails below to scroll through full size images and descriptions).
[fancygallery id=”1″ album=”1″]
Encouraged by the CBCT finding I went back to work with the microscope, ultrasonic, and #6 C+ files and was able to locate the MBII orifice in the middle third of the MB canal. Whew…So the hard part was over. The canals were packed with Calcium hydroxide and we set up another appointment to complete the case on after a few weeks to allow the medication to properly disinfect the canal system.
Mrs. R returned on 2/6/13. Her symptoms were completely resolved and the tooth felt great. I completed endodontic treatment and she was referred back to her general dentist to have the crown repaired. The final x-ray is taken on a distal angulation in order to show all four canals, including he MBII splitting from the MB (Figure 7).
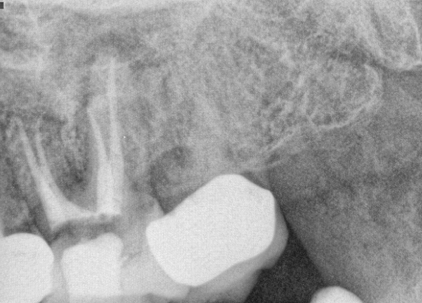
Figure 7: Final Radiograph. Distal angle. MB and MBII canals split in the middle 1/3rd of the MB root and have separate apical termini. The P root periapical bone loss is also evident on this angle.
Mrs. R was a great patient and this was a very challenging and rewarding case!
(Click on thumbnails below to scroll through full size images and descriptions)
[fancygallery id=”2″ album=”2″]
Thanks for visiting Tri City and Falbrook MicroEndodontics.
