How can we allow our patients to see what we see?
As specialists, we have endured the long road of academia, defended our degrees and have the diplomas on the wall to prove that we know a lot about the specialty of Endodontics. But if we cannot explain, convey or inform our patients about their treatment and the technology that is available to them, then we are not practicing at our full potential.
We’d like to take a step back and put ourselves in our patient’s shoes. The focus of this blog is to educate patients about 3-D technology in our practice and how we use it to improve the prognosis of their treatment.
The acronym “CBCT” is an area of confusion for some patients. We often hear similar questions from patients, such as, “What is this? Why do I need it? Can’t you see what you need to see with the film my dentist sent over? I don’t want any more films taken, I don’t want to be exposed to more radiation. Is this going to give me oral cancer? But my pain is up here, why would you want another x-ray on the tooth below it? I just had a Pano, wouldn’t it show up on there? I can’t afford it, can’t we just do the treatment without it?”
Your questions and concerns haven’t fallen on deaf ears.
Perhaps the most important advantage of CBCT in endodontics is that it demonstrates anatomic features in three dimensions that intraoral and panoramic images cannot. CBCT units reconstruct the data to provide interrelational images in three orthogonal planes (axial, sagittal and coronal).

Fig. 1a.
Periapical radiograph of
tooth #30. (1)

Fig. 1b. Sagittal CBCT slice of tooth #30. (1) Note extensive periapical radiolucency
What is it?
The small field-of-view, high-resolution Cone Beam Computed volumetric Tomography (CBCT) unit produces three-dimensional radiographic images of the area in question.
The Kodak 9000 3D system was designed to facilitate better patient care by providing more accurate and dependable treatment planning capabilities at a reduced patient dose.
Patient comfort is also a top priority, which is why the Kodak 9000 3D system features an open, face-to-face design to facilitate patient positioning and allows users to maintain eye contact and ease anxiety. The design and experience is similar to panoramic imaging which most patients are familiar with. The system accommodates patients of all shapes and sizes and is easily accessible to patients in wheelchair.
In general, the use of CBCT in endodontics should be limited to the assessment and treatment of complex endodontic conditions such as:
• Identification of root canal system anomalies and determination of root curvature.
• Diagnosis of dental periapical pathosis in patients who present with contradictory or nonspecific clinical signs and symptoms, who have poorly localized symptoms associated with an untreated or previously endodontically treated tooth with no evidence of pathosis identified with conventional imaging.
• Assessment of treatment complications, such as overextended root canal obturation material, separated instruments, calcified canal identification and localization of perforations.
• Management of trauma, especially root fractures.
• Localization of external from internal root resorption or invasive cervical resorption
• Presurgical case planning to determine the exact location of root apices.

Fig 2. Axial CBCT slice of maxillary left quadrant. Note missed MB2 canal
of tooth #14. (1)

Fig 3a. Periapical radiograph of tooth #20. There is an associated radiolucency at the apex of this root-filled tooth. (1)

Fig 3b. Coronal CBCT slice of the same tooth revealing a missed buccal canal and an associated apical radiolucency. (1)
How does it work?
CBCT is accomplished by using a rotating gantry to which an x-ray source and detector are fixed. A divergent cone-shaped source of ionizing radiation is directed through the middle of the area of interest onto an area x-ray detector on the opposite side of the patient. During the exposure sequence, hundreds of planar projection images are acquired of the field of view (FOV) in an arc of at least 180°. In this single rotation, CBCT provides precise, immediate and accurate 3-D radiographic images. CBCT utilizes a cone shaped x-ray beam and an area detector that acquires a full volume of images in a single rotation, with no need for patient movement.
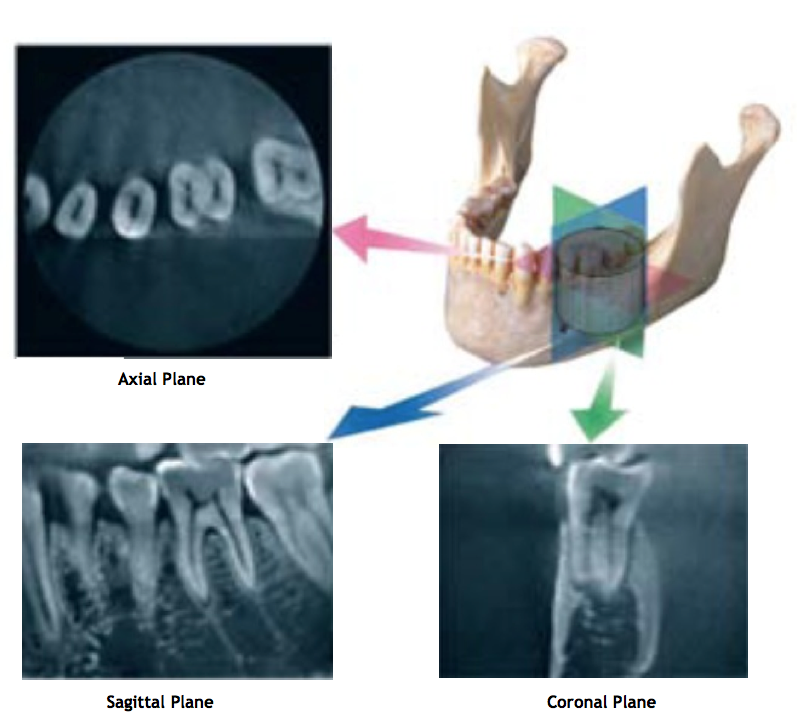
Fig 4. Representation of 3-D view of the lower left quadrant, tooth #19;
axial, sagittal and coronal orthogonal planes. (2)
How much radiation?
Radiation is all around us. It is naturally present in our environment and comes from outer space (cosmic), the ground (terrestrial), and even from within our own bodies. About half of the total annual average U.S. individual’s radiation exposure comes from natural sources. The average annual radiation exposure from natural sources is about 3.1 millisieverts (mSv) or 3,000 microsieverts (μSv).
ALARA is the acronym for As Low As Reasonably Achievable and is a fundamental principle for diagnostic radiology. Clinicians should use CBCT only when the need for imaging cannot be answered adequately by lower dose conventional dental radiography. Computed tomography and CBCT images are composed of a huge volume of data consisting of millions of 3-D voxels. A voxel is a volume element, representing a value on a regular grid in 3-D space. This is analogous to a pixel, which represents 2-D image data. With CBCT data, the voxels are isotropic, meaning they are equal in length, height and depth, which allows for geometrically accurate measurements in any plane.
For a meaningful comparison of radiation risk, radiation exposures are converted to effective dose, measured in Sieverts (Sv). The Sv is a large unit; so in maxillofacial imaging microSieverts [10-6; μSv) are typically reported.
Effective doses for digital periapical radiographs range from 5.5 to 22.0 μSv. Compare this to the annual average dose from background radiation of 3,000 μSv (or 3.0 millisieverts).
The patient dose for 3D CBCT volumes is within the range of one to five regular dental digital periapical radiographs. See the table below to compare CBCTs taken in the anterior or posterior region.
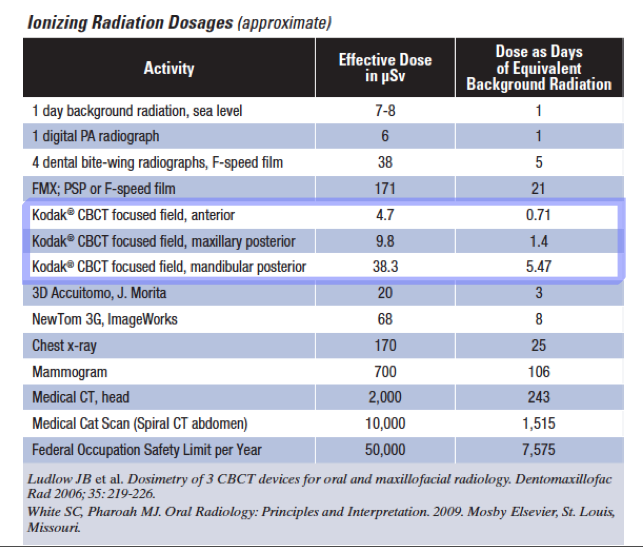
Conventional intraoral radiography provides clinicians with high-resolution imaging that continues to be the front-line method for dental imaging. However, it is clear that there are many situations where the 3-D images produced by the CBCT cannot be disputed. It is a valuable imaging modality, producing minimal radiation exposure to the patient and providing maximal information to the clinician.
Thanks for visiting Tri City and Fallbrook MicroEndodontics.
Special thanks to the following resources:
1. AAE for Figures 1-3 utilized from their Colleagues for Excellence Summer 2011: Cone Beam-Computed Tomography in Endodontics
2. Dr. Christine Peters & Dr. Ove Peters: The Nuts and Bolts of Computed Tomography 2011
3. Ludlow JB et al, White SC, Pharoah MJ. for the table on ionizing radiation dosages
