Case Report of a Silver Point Removal
Silver points were first introduced as an endodontic obturation material in the early 1930’s. At that time and for many decades following, this material was a widely accepted and commonly used material because of their similarity in shape to reamers of the time. Additionally, silver points were easy to use, radioopaque and had mild antibacterial properties. However silver points fell out of favor in the 1960’s as clinicians and researchers came to expect more of obturation materials. Silver points have poor adaptation to canal walls and over time create corrosive byproducts leading to endodontic failure. The AAE (American Association of Endodontics) has put out a position paper on silver point use that can be read here: www.aae.org
Yet despite the adopted principles of the AAE and the endodontic/dental community silver points continued to be placed into the late 1970’s and even early 1980’s. We subsequently see silver points in our office that have existed for a few decades and require retreatment. I suspect we retreat a couple silver point cases per month here at TCF MicroEndodontics. Thus we need to be able to find ways to effectively remove them when needed.
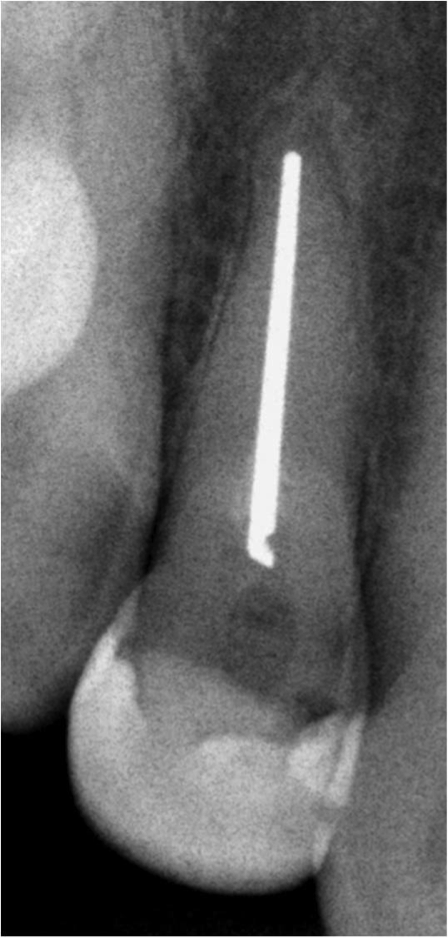
Figure 1: Pre-Operative tooth #7
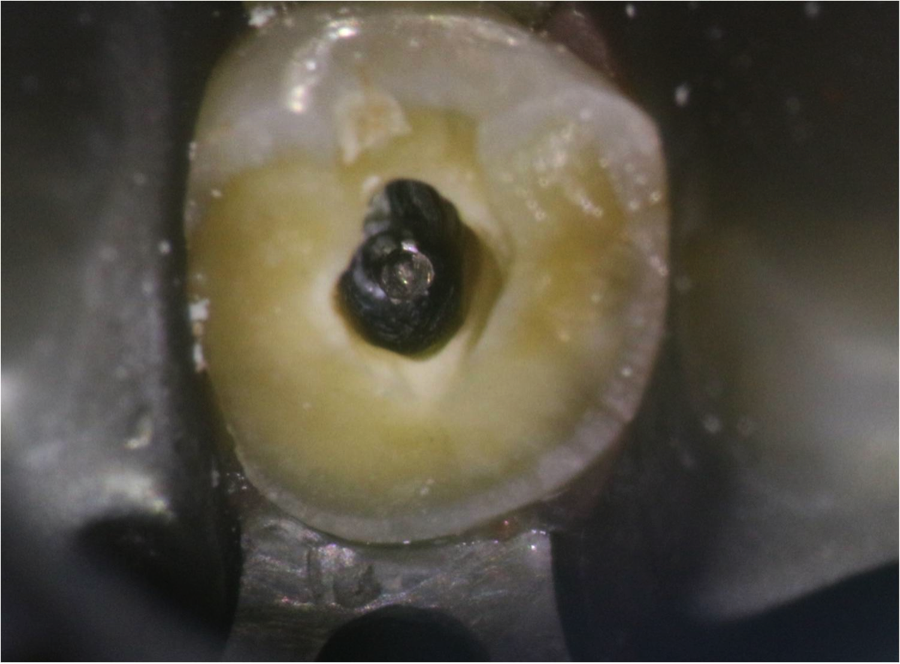
Figure 2: silver point within the root canal
I was presented with this silver point retreatment earlier this week and thought of it as a good case to photograph and share a few ways in which we remove these materials. In this case I used 3 techniques; however there are a few others. When presented with another similar situation, I will document those other approaches in a similar blog post. For this blog I want to cover the following 3 methods: handfile bypass of the silver point, handfile braiding technique, and a composite locking technique.
The pre-operative radiograph (figure 1, 2) shows how tooth #7 broke and that it will require a post/core to retain a new crown. The silver point must be removed to gain that root space for post placement. I started by attempting to bypass the silver point on the buccal and palatal sides. Using small size 6 C-files I engaged the lateral dentin and negotiated the space to reach nearly the full length of the root. Opening this lateral space then subsequently allowed larger files (8,10,15,… files) to fit alongside the silver point. It is preferred to create this lateral space along two sides (in this case the buccal and palatal sides) to help loosen and disengage the silver point from the dentin.
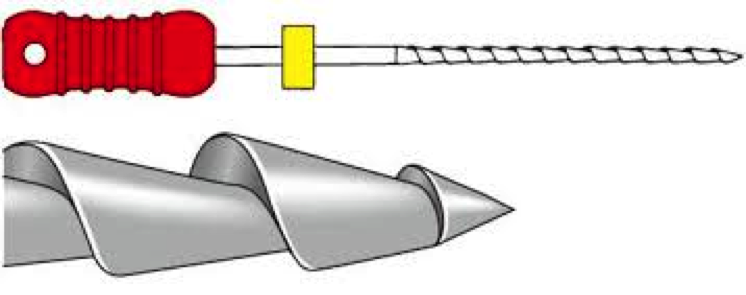
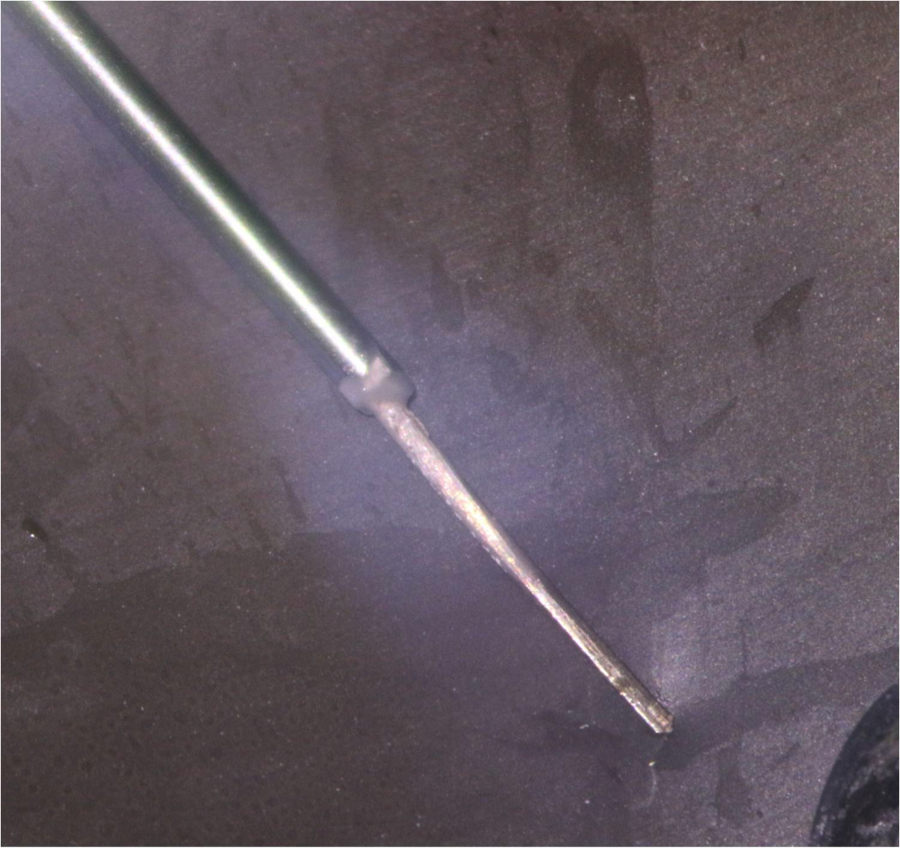
Figure 3: nearly 90 degree rake angle of the hedstrom file
The second method used once there was enough lateral space along two sides of the silver point is to use an H-file (hedstrom file) for a braiding technique. The importance of using H-files is to take advantage of the nearly 90-degree flute angle of this file (Figure 3). This neutral rake angle allows for better engagement of the file along the silver point as compared to a negative rake angle of a standard K or C-file. You will see in figure 4 the H-files are placed on the buccal and palatal sides of the silver point in the same space created from the first method described. The files are then twisted at the file handle causing a spiral tightening of the H-file flutes around the silver point. (Figure 5)
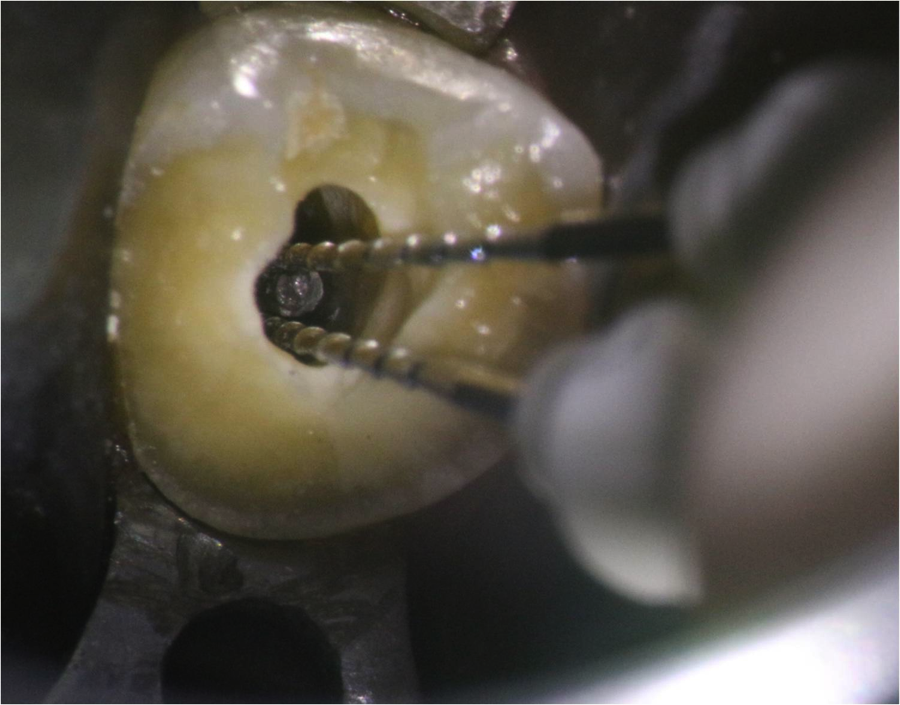
Figure 4: H-files on the buccal and palatal sides of the silver point
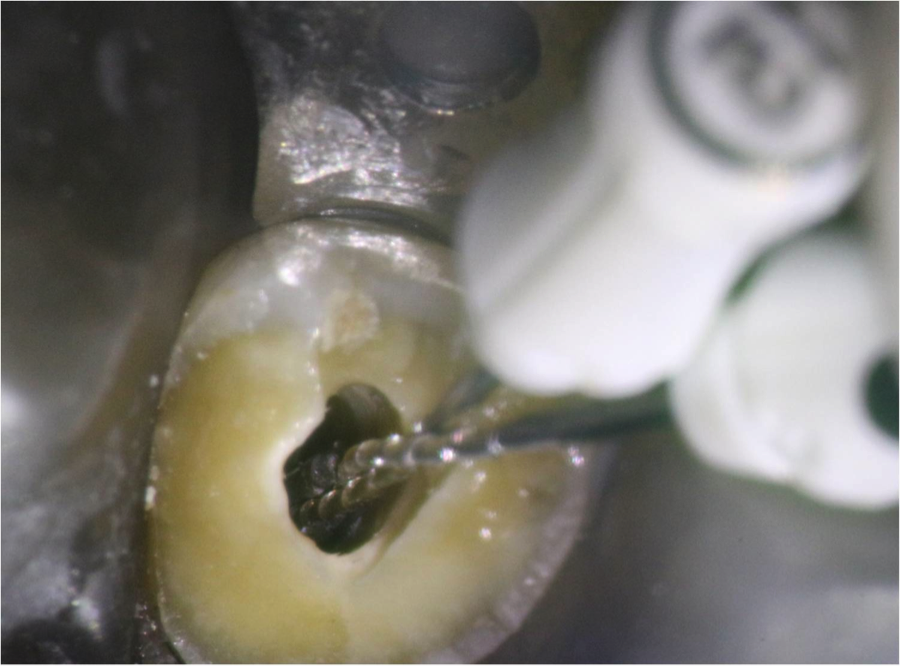
Figure 5: Braiding the H-files by twisting the file handles
The principle is that the fictional force of the files against the silver point will allow us to pull the files and the silver point out at the same time. This is why in order to use this braiding technique we need at least two H-files to bind the lateral surface of the silver point. 3 sides would even be preferred if there is sufficient space.
My many attempts of this braiding technique still did not remove the silver point; however the efforts of the first and second method allowed for enough space in the coronal third of the root to bring me to the next composite locking technique.

Figure 6: Filling the 18-gauge composite applicator tip with a dual-cure composite
Using an 18-gauge composite application tip I delivered composite into the tip so that the stainless steel tube was filled with a dual-cure composite (Figure 6). I then seated the tip of the tube over the silver point as far as possible, which in this case was about 3mm (Figure 7).
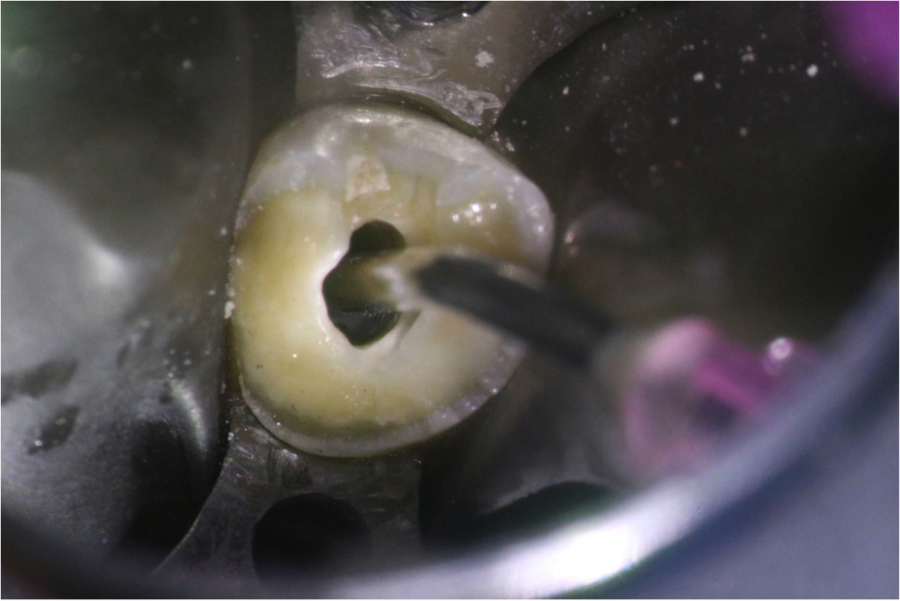
Figure 7: The composite applicator tip fits around the top 3mm of the silver point
The composite cured in about 2 minutes and I simply lifted the composite application tip with the silver point bonded inside (Figure 8, 9). Important elements for this method are to choose a composite applicator tip size that fits over the silver point and covers at least 3mm of the silver point. This will allow for the needed bond strength to lift the silver point out of the canal.
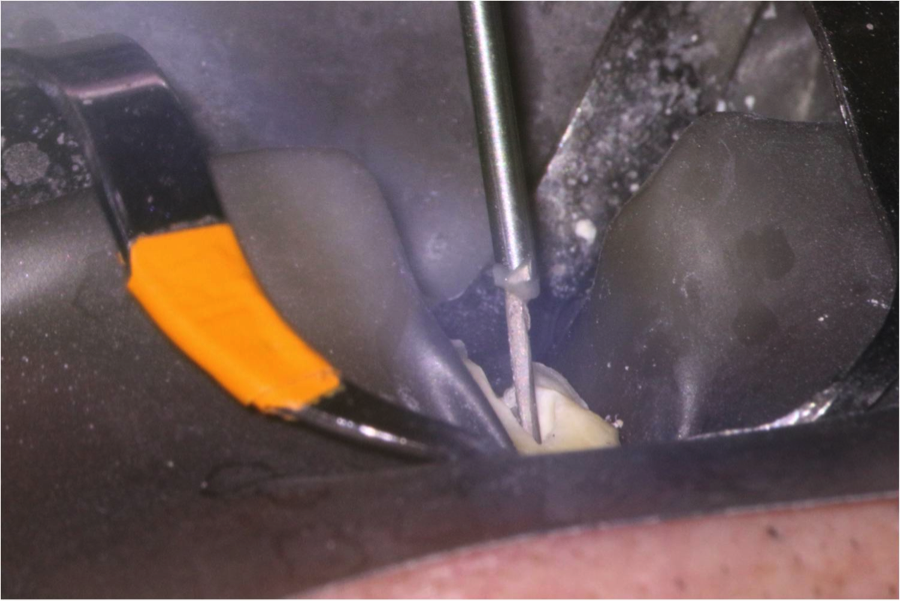
Figures 8, 9 showing the silver point bonded within the composite applicator tip
Once the silver point is removed we simply follow the needed course of cleaning, shaping and obturation that is required of the canal space. Figure 10 is the immediate post-operative x-ray for this case.
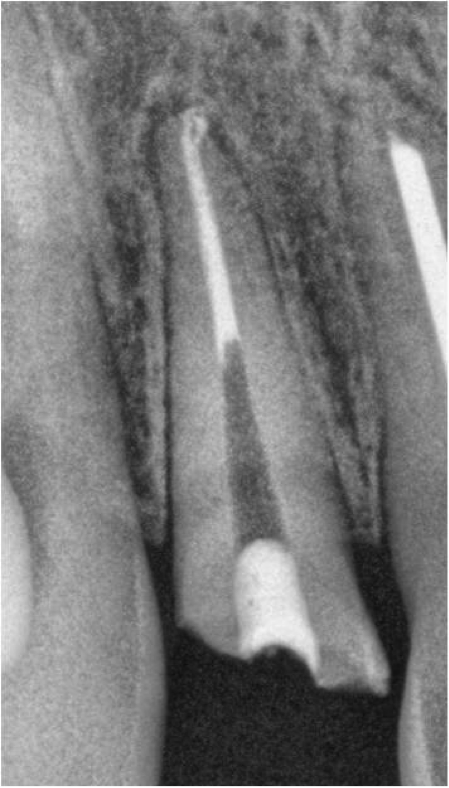
Figure 10: Immediate post-operative #7
Ultimately this treatment resulted in a nice outcome for the tooth and the patient. While we do have a very good success rate of removing such materials, there can be complications or additional challenges with both the material and/or the tooth anatomy not lending itself to these methods. Certainly we will come across future silver points that need retrieval and I will document those cases, their challenges and additional methods we use to achieve great outcomes.
– By Michael Brown DDS