Dental Trauma Part I: Infraction, Crown Fractures and Vital Pulp Therapy
This blog series is dedicated to dental trauma of the permanent dentition, a subject matter that has always been of great interest to me.
As an endodontist, I tend to see a good number of trauma cases per year since many teeth eventually require root canal treatment following injury. Trauma to the teeth and dento-alveolar complex can range from the relatively minor, as with a shallow enamel infraction (crack), or to the severe, as with a tooth avulsion or alveolar bone fracture.
I will include a number of clinical cases that were managed in our office. Other visual aids are borrowed from Traumatic Dental Injuries of the Teeth (4th Ed), edited by J. O. Andreason et al and published by Blackwell Munksgaard in 2007. I oftentimes direct patients and fellow colleagues to www.dentaltraumaguide.org, which is an excellent website operated by the International Association of Dental Traumatology.
In the following part I of the blog, I will discuss crown infraction, crown fractures, and vital pulp therapy.
Crown infraction
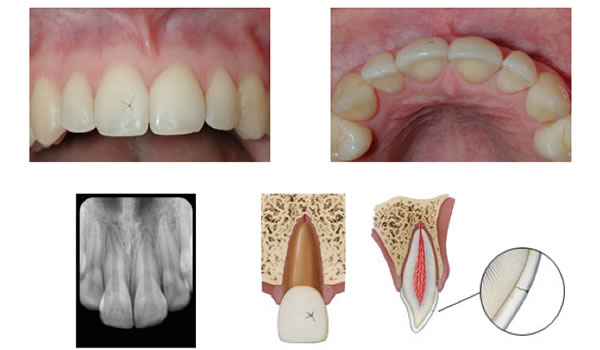
Figure 1. Crown infractions are only evident in a clinical setting. Radiographs will typically not reveal small cracks in the enamel.
An infraction is shallow crack that is entirely contained within the enamel and does not continue into the dentin (Figure 1). There is no loss of tooth structure and very little risk of pulpal inflammation or necrosis. Infractions will unavoidably happen to every single tooth in your mouth given enough time, as they are a natural result of normal wear and tear. I work under a surgical operating microscope on every case and I see infractions all day long. Sometimes they are visible even to the naked eye. Provided vitality testing is WNL, there is no treatment recommended unless the patient expresses an esthetic concern, in which case veneers or crowns may provide a solution.
Crown fracture
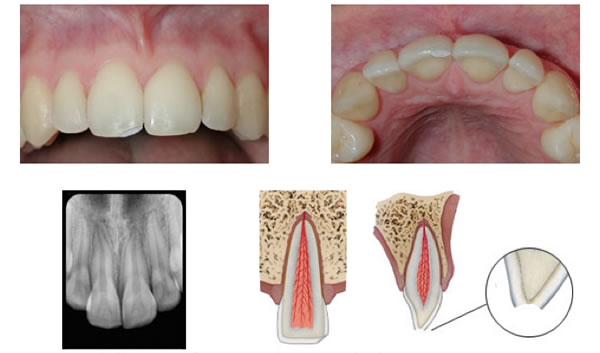
Figure 2. A shallow crown fracture involving enamel only.
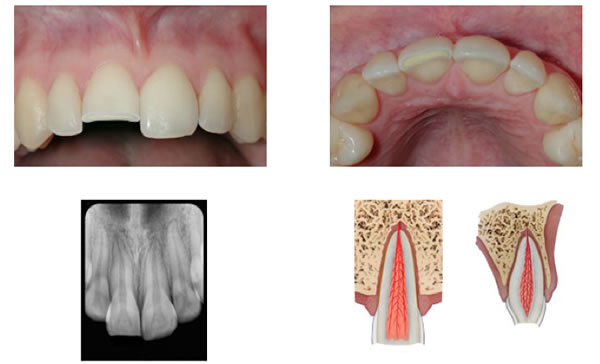
Figure 3. A crown fracture involving both enamel and dentin but without exposure of the pulp.
Crown fractures are the most commonly reported dental injuries, characterized by fractures of the enamel (Figure 2) or enamel and dentin (Figure 3) . There is a loss of tooth structure but no pulpal exposure. The goal of treatment is to close the dentinal tubules to prevent entry of microorganisms and to address patient discomfort. If there is a clean break and the crown fragment is retrieved in tact, it can be simply re-attached to the tooth structure via dentin bonding agents.
The risk of pulpal inflammation and necrosis is generally low but becomes more of a factor if the fracture approaches within close proximity of the pulp. As a general rule, if there is less than 0.5mm of dentin protecting the pulp chamber, it is advised to place a protective glass ionomer liner to close the dentinal tubules, followed by dental adhesives and composite resin. Sealing the dentinal tubules is critical, as it prevents the passage of microbes from the oral cavity into the pulp, which can lead to a strong inflammatory response and eventual pulpal necrosis. GI cements are advantageous as they can also be bonded without etching, which simplifies the clinical procedure and avoids further pulpal inflammation from the conditioning process. The material is also very biocompatible and is oftentimes utilized as a perforation repair or direct pulp capping agent.
Calcium hydroxide cements can be used to line dentin as well however they allow for more microleakage when compared to GI. Additionally, they have been known to disintegrate with time underneath composite fillings and can have a negative effect on resin bonding strength, similar to eugenol based cements.
Complicated Crown Fracture
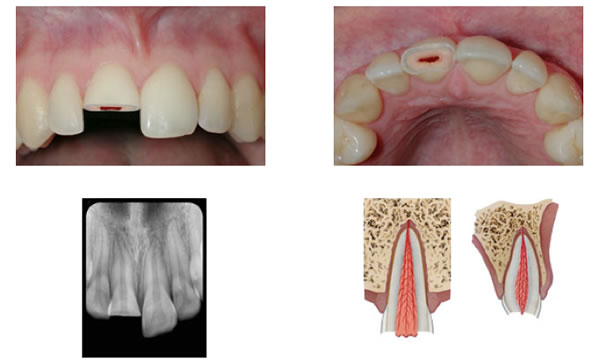
Figure 4. A complicated crown fracture involving enamel, dentin, and the pulp.
Complicated crown fractures involve enamel, dentin, and pulp and pulpal necrosis is imminent without treatment (Figure 4). It is very important for a patient to consult with his/her dentist ASAP in order to allow for the best possible treatment options. Vital pulp therapy (VPT), by way of pulp capping or pulpotomy, is an attempt to maintain the vitality of the pulp tissue and is most successful if attempted ASAP following injury. In mature teeth with closed apices, VPT should be attempted in ideal conditions, however if the pulp cannot be saved, root canal therapy can be performed with a high degree of success. In immature teeth with open apices, VPT should be attempted when at all possible to allow for the continued formation of the root (Apexogenesis). This is extremely important as a tooth with an open apex presents unique challenges for endodontic treatment. The walls are typically divergent at the apex, making proper instrumentation, irrigation, disinfection, and obturation very difficult. Additionally, an incompletely formed root has very thin walls and is at higher risk for fracturing.
Vital pulp therapy
Studies show that within the first 24 hours after a crown fracture and pulp exposure, there is a proliferative inflammatory response that on average involves the most coronal 1.5-2.0mm of the pulp. At this point there is an opportunity to maintain the vitality of the pulp by way of pulp capping. After 24 hours, the chance of success decreases significantly, especially with fully formed permanent teeth closed apices, due to bacterial infiltration deep within the pulp system, and pulpotomy or complete removal of the pulp tissue (root canal therapy) is typically advised.
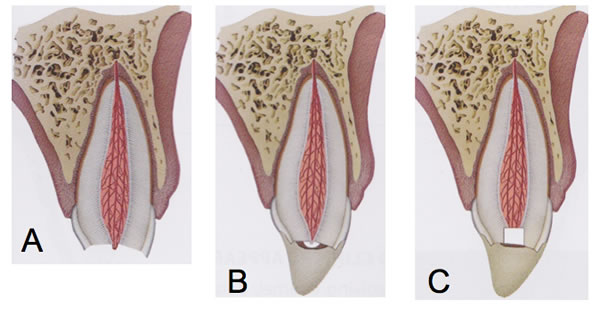
Figure 5. Vital pulp therapy of a complex crown fracture (A) can be achieved via pulp capping (B) or partial pulpotomy (C). The white material pictured directly capping the pulp can be calcium hydroxide, glass ionomer, or MTA.
Pulp capping (Figure 5) is performed by rinsing the exposed pulp tissue with sterile saline and/or chlorhexidine. Sodium hypochlorite, the workhorse of endodontic irrigants, is contraindicated in this circumstance as it will further dissolve the vital tissue that your are trying to save! After proper hemostasis is achieved, the pulp is covered with a small amount of calcium hydroxide, GI cement, or MTA (mineral trioxide aggregate) and then covered with a composite restoration. Ideally the pulp will remain vital and then form a layer of protective tertiary dentin (more specifically reparative dentin) directly beneath the capping material. On a side note…tertiary dentin is simply new dentin that is deposited in response to a caustic stimulus (carious lesion, cavity preparation). This calcified material can be formed by existing odontoblasts (reactionary) or by newly differentiated odontoblast-like cells following the destruction of the original layer of odontoblasts (reparative).
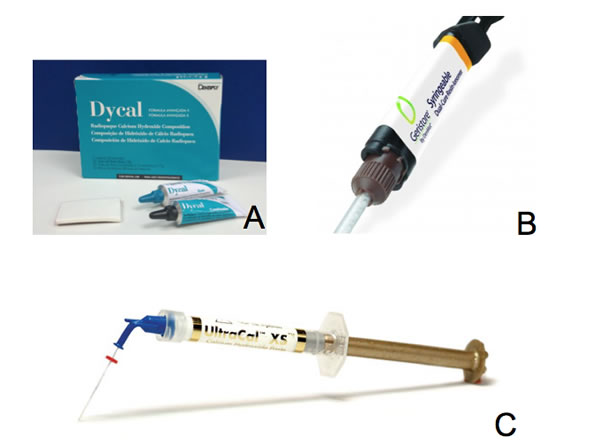
Figure 6. Popular delivery systems for Calcium hydroxide include a hardening paste (A) for pulp capping procedures and a more flowable suspension (C) that can be expressed through a small tip, deep into the root canal system. Geristore (B) is a commonly used glass ionomer cement.
A little more about the materials…Calcium hydroxide (Figure 6) has been used for VPT for decades and certainly has the longest track record. It forms a layer of coagulative pulpal necrosis and kills off bacteria within the pulp to a level of about 1.5-2.0mm apical to its placement. This allows for the practitioner to avoid mechanically removing pulp tissue at all if pulp capping is performed within that 24 hour window (remember at that point pulpal inflammation and bacterial infiltration only extends on average 1.5-2.0mm into the pulp). If successful, repairative dentin will form and the pulp will remain vital. As I mentioned above in the section on crown fractures, glass ionomer cement (Figure 6) is being now used more often than calcium hydroxide because of its similar ability to cause hard tissue formation, while allowing for a better seal.
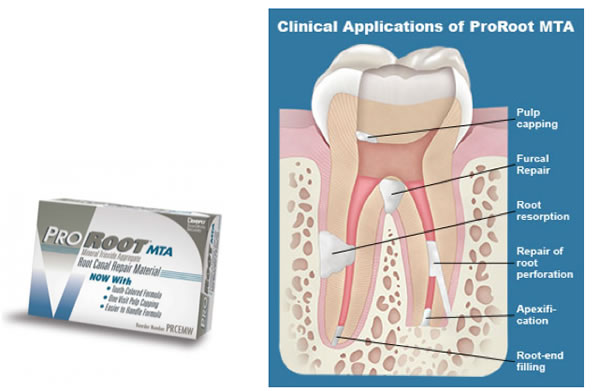
Figure 7. Mineral trioxide aggregate (MTA) is a material we use often with a variety of different clinical applications.
MTA (Figure 7) is arguably the most biocompatible material of the three. It can be used for perforation repairs, pulp capping, resorption repair, apicoectomy retrofills, apexification and obturation of large open apices. I love MTA and use it all the time. In fact my partner Mike Brown and I were recently joking about the incredibly high success rates we get when using the material. MTA may be the “magic pixi dust” of every Endodontist’s armamentarium, however clinical manipulation can be challenging as it resembles wet sand when mixed correctly. Also, the material is hydrophilic and requires a setting time of approximately 2.5 hours in the presence of moisture. We cover MTA with a cotton pellet soaked in sterile water when necessary. Another drawback to MTA is it can stain the coronal tooth structure if used in the pulp chamber or even in the coronal third of the root. This can cause an esthetic concern and require the placement of a veneer or crown.
Back to VPT…A partial pulpotomy (Figure 5), sometimes referred to as a Cvek pulptomy, is a very similar to pulp capping but involves the removal of inflamed pulp tissue to at least 2mm beneath the exposure site in an attempt to reach clinically healthy pulp. This is achieved by using a high speed diamond bur with copious irrigation. Again the pulpal tissue is rinsed with sterile water and/or chlorhexidine until the bleeding has stopped and then covered with one of the three capping agents as previously mentioned. The tooth is then restored with composite. One of the benefits to performing a pulp cap or a partial pulpotomy is that there is typically enough coronal pulp tissue remaining in the pulp chamber to allow for accurate vitality testing during follow-up visits.
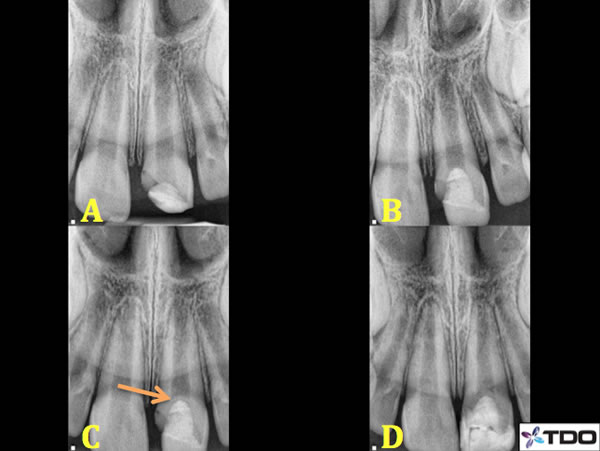
Figure 8. A 7 year old male presented to our office with a complex crown fracture 2 days following a skateboarding accident. His general dentist placed a temporary composite filling over the exposed pulp the day before our consultation although there was no placement of any pulp capping material (A). The roots of 7-10 are immature with open apices. Pulpotomy was performed. I removed the composite filling and 3mm of pulp tissue until reaching healthy pulp. The bleeding was arrested and I placed a layer of MTA, which was allowed to set for a few days prior to covering the material with dual cure composite (B). 4 month recall (C) reveals evidence of a calcific bridge (orange arrow) and continued root formation. Patient remained asymptomatic at the one year recall (D). Further root formation is evident.

Figure 9. A close up of the calcific bridge formation. Immediately after Pulpotomy completed (A) and 4 month recall (B and C).
In the case of immature teeth, an attempt can be made to perform a full pulpotomy (removal of all pulp tissue within the chamber) (Figures 8 and 9) or even a deep pulpotomy (removal of pulp tissue beneath the cemento-enamel junction) in effort to reach healthy bleeding pulp tissue, at which the capping procedure can then be performed.
Again, the ultimate goal of vital pulp therapy is to allow for the formation of a calcific barrier directly beneath the pulp capping material and to maintain pulpal vitality. This is extremely important in immature teeth as you need the pulp to remain vital for the remainder of the root to properly form.
This concludes part I of the series. Part II will follow shortly and will focus on root fractures. Keep in mind, these blogs are meant as an introductory series for a very dense subject matter. If you would like more detail and have any questions please feel free to contact me at Drmonroe@tri-cityendo.com. Thank you for your attention!
Thanks for visiting us at Tri City and Fallbrook Micro Endodontics of San Diego, CA.
