Saving More Teeth! The Periodontic-Endodontic Infection
Lateral root and furcation lesions can be tough to deal with indeed.
There is so much more to consider from a diagnostic and prognostic perspective than in the typical periapical radiolucency. We have to think about vertical fractures, periodontal abscesses, combination endodontic/periodontal infections; and if a combination lesion, is this primary endo or primary perio. There are other possible cysts found between roots that fall outside of the pure scope of endodontics as well. Thus needless to say when we come across a lateral root or furcal radiolucency we take a more guarded approach to diagnosis and treatment options.
The ultimate question is whether or not the infection will resolve with endodontic therapy. Certainly we only wish to provide treatment to conditions we can resolve predictably. Very unpredictable conditions will be better served with implants or bridgework. But despite our goal of providing predictable endodontic treatments, these conditions of lateral root or furcal infections are not always black and white. And because of some grey area we must take into account other factors that are not directly related to the tooth such as patient motivation, their time, and their willingness to proceed with a treatment that could be prognostically questionable.
We have found though that there are ways to minimize the uncertainty in the prognosis. We have also found that there are so many lateral root lesions or furcation lesions that will heal by endodontic treatment. I would now recommend endodontic treatment and expect a reasonable success rate on many of these teeth that perhaps 5-7 years ago I might have condemned for extraction. Understanding the reasons for lateral root lesions is critical, but also just developing an intangible and unteachable gut feeling on when or when not to treat endodontically carries a lot of weight. That gut feeling is perhaps the more challenging thing to write about. So let’s start with the more common reasons for lateral root lesions to be even present.
Let me first point out some of the main reasons when this type of infection can heal by conventional endodontic therapies:
–lateral lesion caused by a lateral canal that harbors bacteria (figure 1)
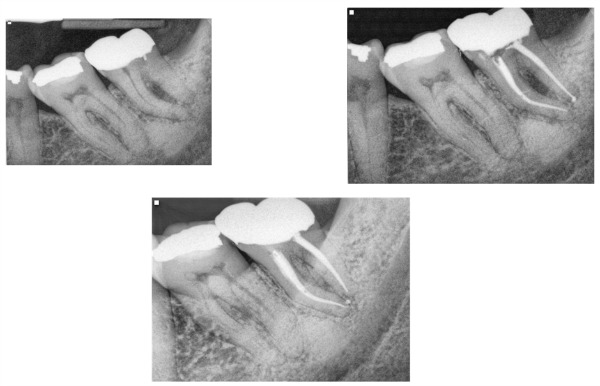
Fig.1 Here is a case of a furcal lesion treated by Dr. Michael Sherman. In the radiograph in the upper right you can see a small lateral canal on the mesial root communicating with the furcation. That lateral canal is filled with sealer and the 2 year recall shows excellent healing.
–lateral / furcal lesion caused by a primarily endodontic infection that creates the lateral and periodontal defect (figure 2,3)
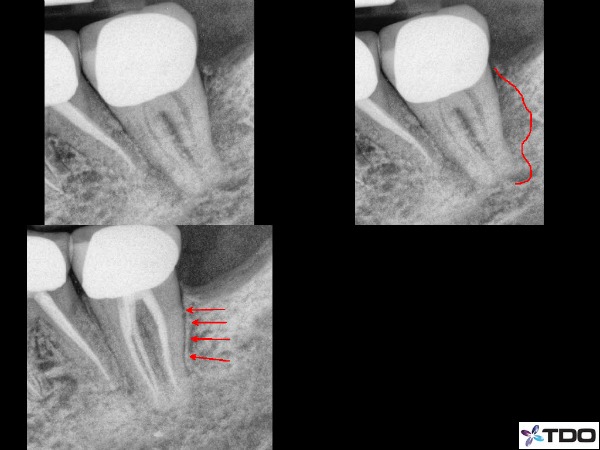
Fig.2 Here is a case I treated about 1.5 years ago. The illustration shows the significant lateral and distal bone loss on the distal root of #18. The 8 month recall is on the bottom left side with red arrows showing excellent bone healing. This tooth went from a 2 mobility to rock solid before I had completed the case with 2 months of CaOH in the canals.

Fig. 3 This was a retreatment case by Dr. Sherman in which he medicated the canals over 3 appointments using CaOH. The upper left is the pre-operative x-ray. Upper right is the immediate post-operative x-ray and the lower x-ray is the 1 year recall. There has been significant bone fill into the furcation which will continue to improve over time.
Conditions of lateral infections that will not resolve by endodontic means are commonly:
–vertical root fractures (figure 4)
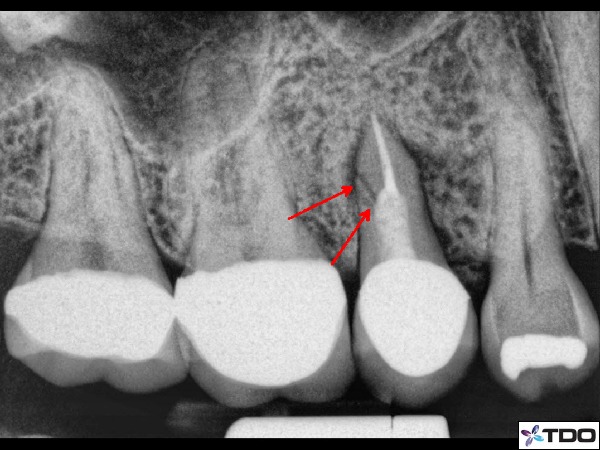
Fig. 4 Clear vertical root fracture illustrated with red arrows. Note: it is rare to see radiographic confirmation of a fracture.
–periodontal disease (periodontitis) (figure 5)
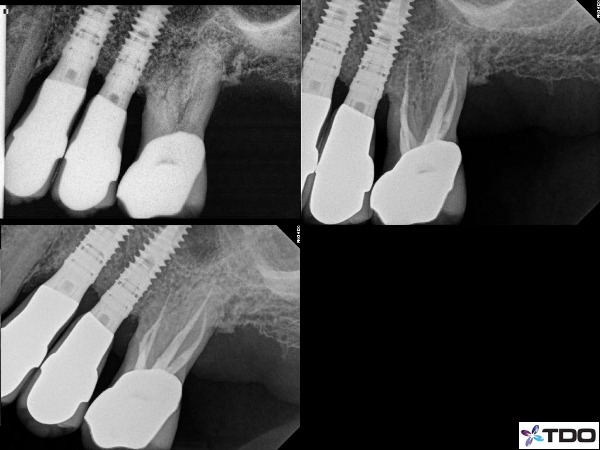
Fig.5 This is a case that needed endodontic treatment, but also had the a separate issues of periodontal disease resulting in horizontal bone loss. I do not believe in this case one problem was contributory towards the other. He had generalized horizontal bone loss around all of his teeth. I performed the RCT and the lower right is a 6 month recall. The patient remains asymptomatic.
–periodontal abscess
–a few other odontogenic / non-odontogenic cysts, tumors, etc (not to be discussed in this blog)
Conditions that may or may not require endodontic intervention:
–external root resorptive defects (figure 6)
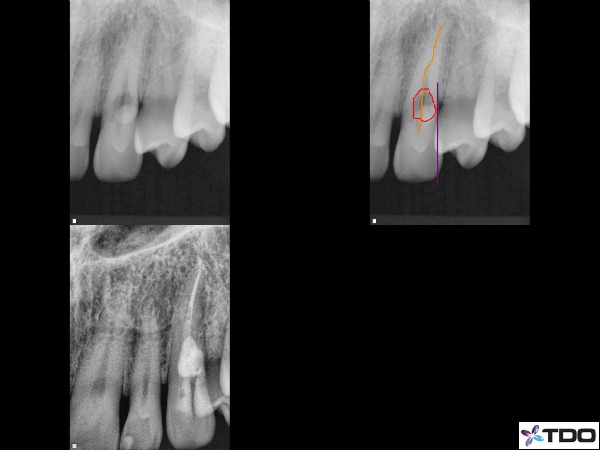
Fig.6 This tooth was referred for evaluation with a moderate degree External Cervical Invasive Resorption process on the buccal surface. There was initially a 9mm buccal probing with associated buccal bone loss. I performed RCT and then surgically entered the site to repair the defect with Geristore. At our 1 month check-up the sulcus depth was restored back to 4mm.
–horizontal root fractures (depending on location tooth may or may not be saved) (figure 7)
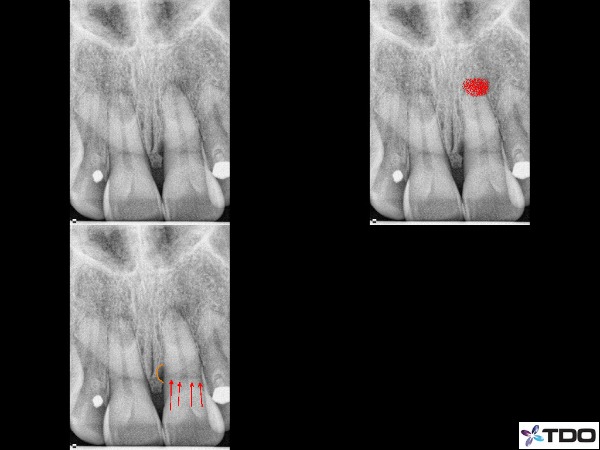
Fig.7 This lateral root lesion appears near the crestal bone level on the mesial side of tooth #9. The illustrations in orange and red show the lesion and a horizontal root fracture.
The often difficult part is in the diagnosis. Of the above set of conditions we need to have a good indication for the etiology of the infection in order to communicate to our patient the issues, the treatment options, and the pre-operative prognosis. However, sometimes it is just not that easy to explain as there are so many factors contributing to the diagnosis. Taking into account the periodontal condition is the first step. We must find out the sulcus depth, width of defect, how many bony walls remain mobility, and periodontal status of the rest of the mouth. Generally speaking the more advance the periodontal condition the less predictability in saving the tooth (this is not a hard-line rule though as we have successfully treated many teeth of advance mobility). Testing the pulpal condition is next. This will help to determine a true endodontic component so that we can then build evidence to suggest a relationship between the lateral/furcal radiolucency and the pulp condition. Many times lateral or furcal lesions have no endodontic involvement at all. These conditions can be treated via periodontal intervention or extraction.
Using the microscope is critical as well. We will look for fractures on the tooth surface. Even on crowned teeth we can tease the sulcular tissue back and see tooth surface to inspect for fractures. The diagnosis phase can extend into the actual treatment phase as well. It is not uncommon to access a tooth and shape the coronal third of a canal to find/inspect the depth of a fracture. In fact, we feel this is often the best way to diagnosis a vertical root fracture. Visualization will lead to a more confident treatment recommendation. In our office I suspect we will investigate deeply for a fracture at least once per day. Again this is still part of the diagnostic phase.
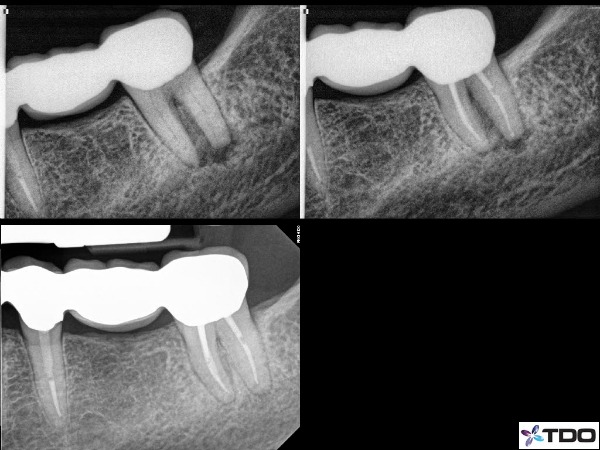
Now that we have CBCT imaging in the office we can use that additional and valuable tool. However, one thing to be aware is that the CBCT will rarely show a vertical fracture. Our CBCT machine will allow us to view individual slice thickness as small as 0.076mm, but most fracture lines are even smaller in width. However, it does show the bone loss patterns. We can look for vertical bone loss that is not present on the regular periapical x-ray. We can look for a narrow site of vertical bone loss (figure 8). Vertical sites of bone loss in near proximity to posts are also quite suggestive of a fractured root. Areas of radiolucency that is only present on a lateral surface vs. infections that have an apical presence with a lateral presence. These would be helpful indicators to determine if the presence of a fracture and ultimately if a tooth is savable.
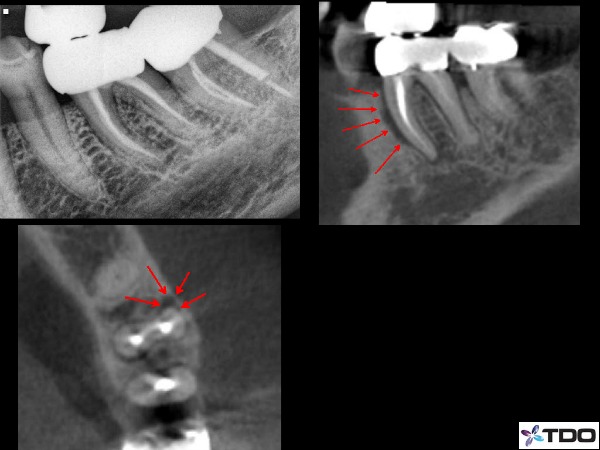
Fig.8 This patient arrived with pain localized to tooth #19. The periapical radiograph does not show anything definitive. However the CBCT certainly shows a long, narrow, and localized pattern of bone loss on the MB line angle of the mesial root. This would certainly be quite suggestive of a root fracture.
Finally there is the “gut feeling” of whether a tooth is savable or not. This is not scientific and it is variable. But I really feel it is worthy of discussion despite there being no real teaching method to a “gut feeling” approach. Anyone who has practiced (dentistry or medicine) for years will see conditions that are not necessarily discussed in a textbook. And over time we will learn how to deal with them better. This is developed over years of treating teeth and experiencing similar scenarios (figure 9). Admittedly though my gut feeling may sometimes be different than someone else. Even here in our office I might have some different interpretation of a case than my partners. But that is also one big advantage that I feel in working with my partners. In diagnostically challenging situations always talk about it together to gain another perspective that could prove very valuable. Everyday we share cases and gain perspectives from each other.
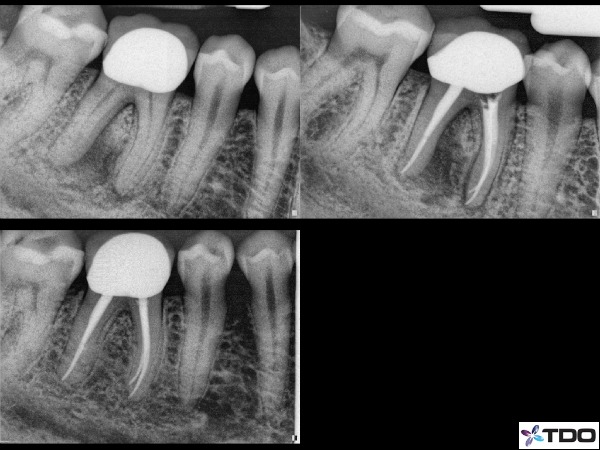
Fig.9 Here is a case done by Dr. Adam Monroe on 3/1/11. This tooth did have a deep probing near the apex on the distal root. Over the course of 3 appointments and using CaOH for 2 months the probing decreased to a normal 4mm and the 1.5 year recall shows excellent bone fill.
Treatment approach for conditions of lateral or furcal radiolucency
There are a lot of factors that come in to play during the treatment phase. Furthermore, not all treatments initiated are necessarily completed. Each step of the way there are bench marks that must be met in order to progress to the next step. These bench marks can be case specific, but I will discuss just a generalized approach.
Once we have decided to treat a tooth and have some expectation of saving this tooth we will always take a multi-visit approach. This is a minimum of 2 appointments and can be 3 or more in some cases. The reason for this is to use calcium hydroxide (CaOH2) as an intracanal medicament to kill bacterial cells. We typically always use CaOH in any infected tooth, but it becomes even more important for cases with any question mark on the long term prognosis. Anything we can offer to increase our chances of success we will do.
Additionally, we will allow the medicament to remain for at least 3 weeks between appointments and often upwards of 4 weeks. At the second appointment we will check for symptoms or signs of improvement before deciding to complete a case. Is the patient asymptomatic? If a pre-operative fistula was present, has it resolved? If there was initially a deep sulcus depth, has that depth reduced significantly? If there was advanced mobility, has that reduced significantly? All of these conditions need to be met in order to complete the case. (figure 10) If there has not been enough progress then consideration for reinstrumentation and remedicating with CaOH for another month is appropriate with the same reassessment at the next visit. If symptoms or signs have become worse than reconsideration for endodontic therapy vs. extraction is appropriate. Controlling these factors before treatment is complete is huge advantage to the multi-visit process. Additionally, there is also so much value to this approach from the patient perspective. Even in situations that end with extraction. Our patients feel that we did everything we can and they appreciate it so much.
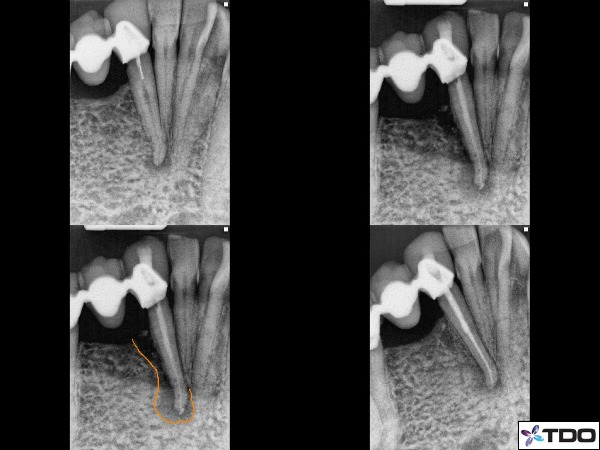
Fig.10 This was a unique case in which the patient came with an original condition shown in the upper left x-ray. She did not return to our office for treatment until 7 months later with swelling, pain, class 2 mobility, and a deep distal root probing to the apex. The x-ray of the upper right side shows the lateral bone loss with CaOH in the canal. I had put CaOH in this canal for 2 months over the course of 3 appointments. The orange line shows the amount of lateral bone loss.
The final radiograph in the lower right shows reconstitution of the ligament space in just two months. The probing had reduced to 5mm and very little mobility.
Of course during treatment we will continuously look for signs that might change our opinions of a tooth for better or worse. We will look for fractures and fracture depth, resorptive conditions, accessory anatomy, etc. Finally, once the treatment has been completed we will track these teeth closer than we do most. So for us we will recall the patient every 3 months.
In the end, I think what I would most like to communicate is that there really are a lot of lateral or furcal radiolucent conditions that can heal. It takes knowledge of why these lesions exist and a careful approach to diagnosis and treatment. We are not a 100% right and we cannot give guarantees, but we can certainly minimize the chances of misdiagnosis and/or failing endodontics if we spend some extra time analyzing and looking for the signs of improvement before completion of treatment. Going the extra lengths to save a tooth can be quite rewarding. You will save more teeth than you might have once thought was possible.
The presentation of this case was that of a buccal fistula just below the free gingival margin and deep isolated probing into the furcation. Tooth was treated over 2 visits with one month of calcium hydroxide. The fistula had healed and the probing reduced to 4mm at the buccal furcation. Completion appointment x-ray in the upper right. X-ray at the lower right is the 5 month recall showing excellent furcal bone fill.
Thanks for visiting Tri-City and Fallbrook MicroEndodontics.
